Diabetic Foot Ulcer DFU Treatment Market to Witness A Pronounce Growth During 2023-2026
Table of Content
Your doctor may prescribe antibiotics, antiplatelets, or anticlotting medications to treat your ulcer if the infection progresses even after preventive or antipressure treatments. An infection is a serious complication of a foot ulcer and requires immediate treatment. Poor blood circulation is a form of vascular disease in which blood doesn’t flow to your feet efficiently.

The evidence for special footwear to treat foot ulcers is poor but their effectiveness for prevention is well-established. Design features of footwear that are effective in reducing pressure are arch supports, cushioned cut-outs around points at risk of damage, and cushioning at the ball of the foot. Technology for measuring the pressure within the shoes is recommended during designing diabetic footwear. Steps to prevent diabetic foot ulcers include frequent review by a foot specialist and multidisciplinary team, good foot hygiene, diabetic socks and shoes, as well as avoiding injury. Foot-care education combined with increased surveillance can reduce the incidence of serious foot lesions. Papanas N, Maltezos E. Benefit-risk assessment of becaplermin in the treatment of diabetic foot ulcers.
What Is A Diabetic Foot Ulcer
Moreover, it has been reported that local concentrations of growth factors [platelet-derived growth factor-beta (PDGF-beta), transforming growth factor-beta] are low in patients with chronic ulcers . Various dressings are available that are intended to prevent infection and enhance wound healing, and several studies support their effectiveness for this purpose . However, most of these studies were performed in wounds and not in diabetic ulcers .
There is strong evidence that fibroblasts, endothelial cells, and keratinocytes are replicated at higher rates in an oxygen-rich environment . Moreover, leukocytes kill bacteria more effectively when supplied by oxygen. It is also known that fibroblasts from diabetic individuals show diminished cell turnover in comparison with those from nondiabetic persons. Based on these data, the idea was that the administration of oxygen at high concentrations might accelerate wound healing in diabetes .
Guidelines For The Use Of Adjuvant Agents In The Treatment Of Diabetic Ulcers
Continuous pressure on the skin tightens the blood vessels, which are responsible for providing nutrients and oxygen to the skin. When the skin is too long anemic, tissue will die, causing the formation of pressure ulcers. Also known as bedsores or decubitus ulcers, pressure ulcers are a common skin condition people have to cope with.

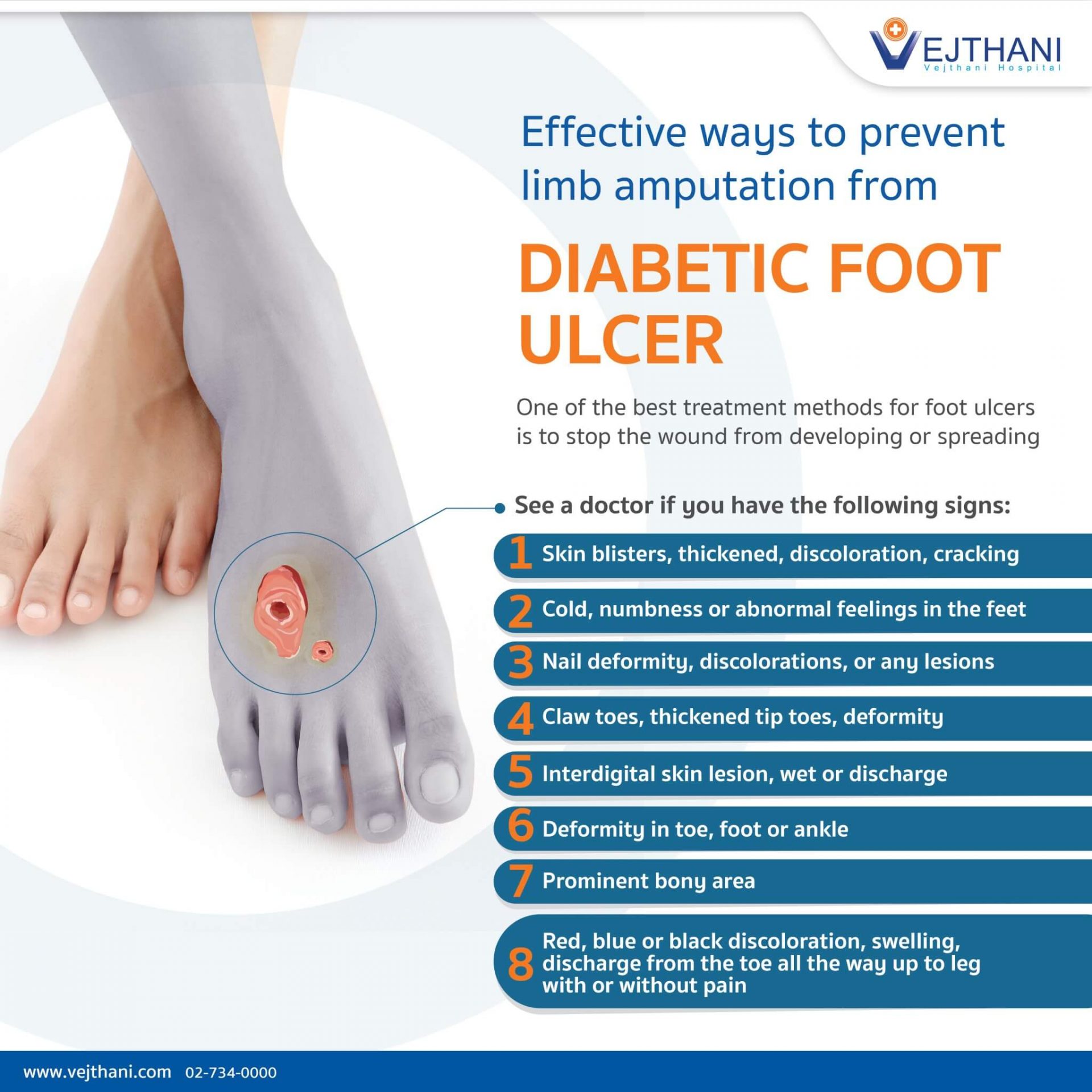
Research, however, has shown that the development of a foot ulcer is preventable. Ulcers on the feet are particularly common in those who have diabetes. Complications from the disease – such as poor circulation and loss of feeling in the feet due to diabetes-related nerve damage – make it more likely for a wound to develop, and also harder to heal. Remaining on a diet that helps you meet your glycemic targets and off-loading pressure from your feet is the most effective way to allow your foot ulcers to heal. While your ulcers heal, stay off your feet and follow your treatment plan. If you begin to see blackened flesh around an area of numbness, see your doctor right away to seek treatment for an infected foot ulcer.
Wear wide soled shoes
The International Working Group on the Diabetic Foot has issued an evidence-based guideline which lists out the principles of ulcer treatment. As per IWGDF, foot ulcers will heal in the majority of patients if the clinician bases treatment on the principles outlined. Patients with an ulcer deeper than the subcutaneous tissues may require intensive treatment and in some cases need to be hospitalised. Adjunctive systemic hyperbaric oxygen therapy in treatment of severe prevalently ischemic diabetic foot ulcer. Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, Lavery LA. Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients. Lavery LA, Armstrong DG, Vela SA, Quebedeaux TL, Fleischli JG. Practical criteria for screening patients at high risk for diabetic foot ulceration.

Vascular ulcers are caused by problems with the vascular system . Sometimes, you won’t even show symptoms of ulcers until the ulcer has become infected. If a foot ulcer has become infected, a doctor prescribes antibiotics. This medication is usually taken by mouth and fights infection by killing bacteria. The length of time you need to take the medication varies based on the extent of the infection.
DFUs are identified to come with a continued inflammatory response plus extracellular matrix irregularity. Collagen dressing companies support and formulate a scaffolding model that controls extracellular components, consequently moving chronic injuries toward closure. Otherwise, the panel encourage the inclusion and capture of different dressing types in High Risk Foot Service database monitoring systems to benchmark the different dressing typesâ efficacy on local DFU healing. While you may have heard that itâs important to âair outâ wounds, experts now know that not covering a wound actually increases the odds of infection and slows healing. If you do get an ulcer or notice a change in your skin that youâre not sure about, tell your doctor right away. Youâll likely get a procedure called debridement, which removes unhealthy tissue from the wound to spur healing.

Stem cell therapy may represent a treatment for promoting healing of diabetic foot ulcers. Investigations into characterizing and identifying the phyla, genera and species of nonpathogenic bacteria or other microorganisms populating these ulcers may help identify one group of microbiota that promotes healing. Approximately 15 percent of people with diabetes experience foot ulcers, and approximately 84 percent of lower limb amputations have a history of ulceration with only approximately half of amputees surviving for more than 2 years. 56 percent of individuals with foot ulcers who do not have an amputations survive for 5 years. Foot ulcers and amputations significantly reduce the quality of life. Approximately 8.8 percent of hospital admissions of diabetic patients are for foot related problems, and such hospital admissions are about 13 days longer than for diabetics without foot related admissions.
There is low-certainty evidence that negative pressure wound therapy would improve wound healing in diabetic foot ulcers. Diabetic foot ulcers should be carefully evaluated and the gold-standard treatments should be strictly applied in order to prevent amputation. Accumulating evidence shows that bioengineered skin substitutes may be a promising therapeutic adjunct therapy to the standard wound care for the management of noninfected diabetic foot ulcers. Nevertheless, more studies need to be conducted in the future in order to confirm these results [63–69].

Autolysis is enhanced by the use of proper dressings, such as hydrocolloids, hydrogels, and films. Autolysis is highly selective, avoiding damage to the surrounding skin . Medical trial data confirmed that becaplermin benefits in reducing the danger of amputation, plus more than one-third DFUs treated in the existing group with regular RH PDGF-BB Vs. The Placebo limitation group. At week 20.1, Becaplermin has been confirmed to contribute a 43% greater healing rate for neuropathic ulcers than a placebo gel.
Members of the expert panel were provided a conflicts of interest disclosure statement from IDSA and were asked to identify ties to companies developing products that might be affected by promulgation of the guideline. The statement requested information regarding employment, consultancies, stock ownership, honoraria, research funding, expert testimony, and membership on company advisory committees. The panel was instructed to make decisions on a case-by-case basis as to whether an individual’s role should be limited as a result of a conflict, but no limiting conflicts were identified. Ehrenreich M, Ruszczak Z. Update on tissue-engineered biological dressings. Williams DT, Harding KG, Price P. An evaluation of the efficacy of methods used in screening for lower-limb arterial disease in diabetes.
Simply walking each day can help prevent the leg ulcer from getting worse and reduce the amount of swelling you experience in your legs. Be sure to wear shoes that do not put a lot of pressure on only one part of your foot. HealthTap doctors are based in the U.S., board certified, and available by text or video. If you have concerns with any of the above, please get in touch with your healthcare professional for advice. Find a well-lit area, perhaps under a lamp or in the bathroom, and look closely at your entire foot especially the tips of your toes and the bottoms of your feet. If you aren’t able to see your feet, ask a family member or caretaker to check them for you.
Effect of topical basic fibroblast growth factor on the healing of chronic diabetic neuropathic ulcer of the foot. Yönem A, Cakir B, Güler S, Azal OO, Corakçi A. Effects of granulocyte-colony stimulating factor in the treatment of diabetic foot infection. Enhanced skin wound healing by a sustained release of growth factors contained in platelet-rich plasma. Pound N, Chipchase S, Treece K, Game F, Jeffcoate W. Ulcer-free survival following management of foot ulcers in diabetes. A systematic review of interventions to enhance the healing of chronic ulcers of the foot in diabetes.

Metabolically altered collagen is known to be highly inflexible and prone to break down, particularly over pressure areas. Fibronectin is the major glycoprotein secreted by fibroblasts during initial synthesis of extracellular matrix proteins. It serves important functions, being a chemo-attractant for macrophages, fibroblasts and endothelial cells. The cells break down damaged ECM and replace it, generally increasing in number to react to the harm. The process is activated, though perhaps not exclusively, by cells responding to fragments of damaged ECM, and the repairs are made by reassembling the matrix by cells growing on and through it. Because of this, extracellular matrix is often considered as a 'conductor of the wound healing symphony'.
Comments
Post a Comment